PDC: PICU Data Collaborative
The adoption of electronic medical record (EMR) systems is generating a deluge of clinical data, but large amounts of high quality data are neither readily nor widely available to researchers. Datasets used by various groups and studies remain siloed, which makes it difficult to make ‘apples-to-apples’ comparisons of results from emergent AI methods. Additionally, the low prevalence of specific critical care syndromes means that any one particular unit has limited ability to establish sufficiently large cohorts of patients for robust clinical research. The Pediatric Data Collaborative (PDC) was formed to address these challenges by developing a rich, curated, standardized, multicenter data source. By doing so, it will promote the discovery and application of knowledge to improve the diagnosis, prognosis, and treatment of critically ill children. Since its inception in 2019, the PDC has grown to include 19 major pediatric institutions across the nation and is the largest collection of high-resolution time-series pediatric critical care data. The VPICU leads the infrastructure development for this collaborative. More information can be found at https://pedsdata.org/

ML-ROVER: ML to Reduce Laboratory Test Overutilization
Many laboratory tests are unnecessary and contribute to reduced care quality. Funded by a NIH R21 grant, the VPICU is using the rich, multisite data from the PICU Data Collaborative to develop machine learning models that forecast future laboratory values in critically ill children and identify processes to use these forecasts to reduce laboratory overutilization. Further, this collaborative project will apply user-centered design principles to develop clinical decision support tool(s), deploy the tool(s) at a pilot site, and establish the groundwork for a future effectiveness-implementation trial.
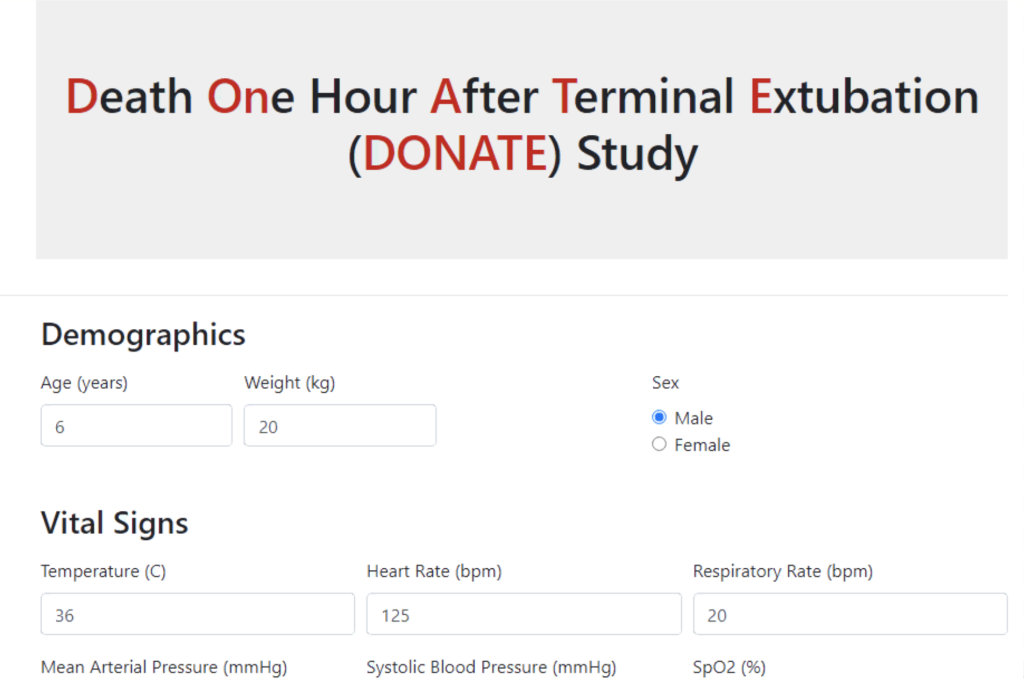
DONATE: Predicting Death within One Hour After Terminal Extubation
This project aims to develop an AI application to augment family counseling and identify suitable candidates for organ donation after cardiac death (DCD) by predicting Death within One Hour After Terminal Extubation (DONATE). What started as a single site study has grown to a 10-site study, with 9 other institutions joining CHLA, led by Dr. Meredith Winter, a CHLA pediatric intensivist. The first phase of the multisite study developed and validated, both externally and temporally, a machine learning model to predict death within one hour after terminal extubation. The second phase will expand model validation (new sites and different operational scenarios), develop a clinical decision application, and gather user feedback to maximize its clinical impact.
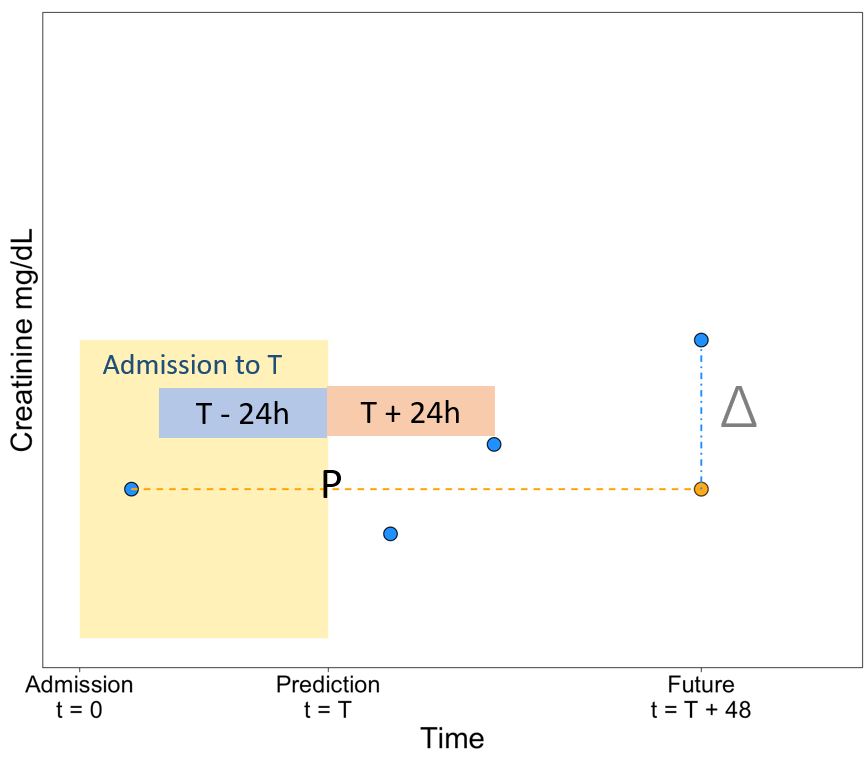
Predicting Creatinine Clearance in Critically Ill Children
Vancomycin is commonly used as a broad-spectrum treatment for bacterial infections. While effective, it is also nephrotoxic (harmful to the kidneys). Overdosing can lead to toxicity or irreversible Acute Kidney Injury, while under-dosing may reduce the drug’s effectiveness. Currently, vancomycin is administered using standard or uniform dosing, which assumes that a patient’s condition remains stable from day to day. If clinicians had the ability to predict a patient’s future renal function, they may be able to dose vancomycin more precisely, ensuring it is effective without compromising kidney health. Supported by an NIH RO1 grant, the VPICU is collaborating with Dr. Michael Neely, Chief of CHLA’s Division of Infectious Diseases to predict the future renal function of critically ill children for more precise drug dosing.
Detection of Patient-Ventilator Dyssynchrony
Invasive mechanical ventilation is frequently life saving for patients with respiratory failure but has significant risks. Patient Ventilator Dyssynchrony (PVD) occurs when there is a mismatch between a patient’s respiratory effort and the support provided by the ventilator. Collaborating with Dr. Robinder Khemani, Vice Chair of Research in ACCM at CHLA, and Dr. Benjamin Yoon, previously a Critical Care Medicine Fellow at CHLA and currently a pediatric intensivist at Children’s Hospital Colorado Anschutz, the VPICU developed models to detect PVD from ventilator waveform data. With support from an NIH RO1 grant, this project has evolved into an international collaboration involving prospective data collection at four institutions to characterize PVD in relation to clinical and mechanical outcomes of ventilated children. The VPICU is continuing to develop its PVD models to enable the annotation of large, high-resolution datasets and support the development of a clinical decision support application for real-time bedside detection of PVD.
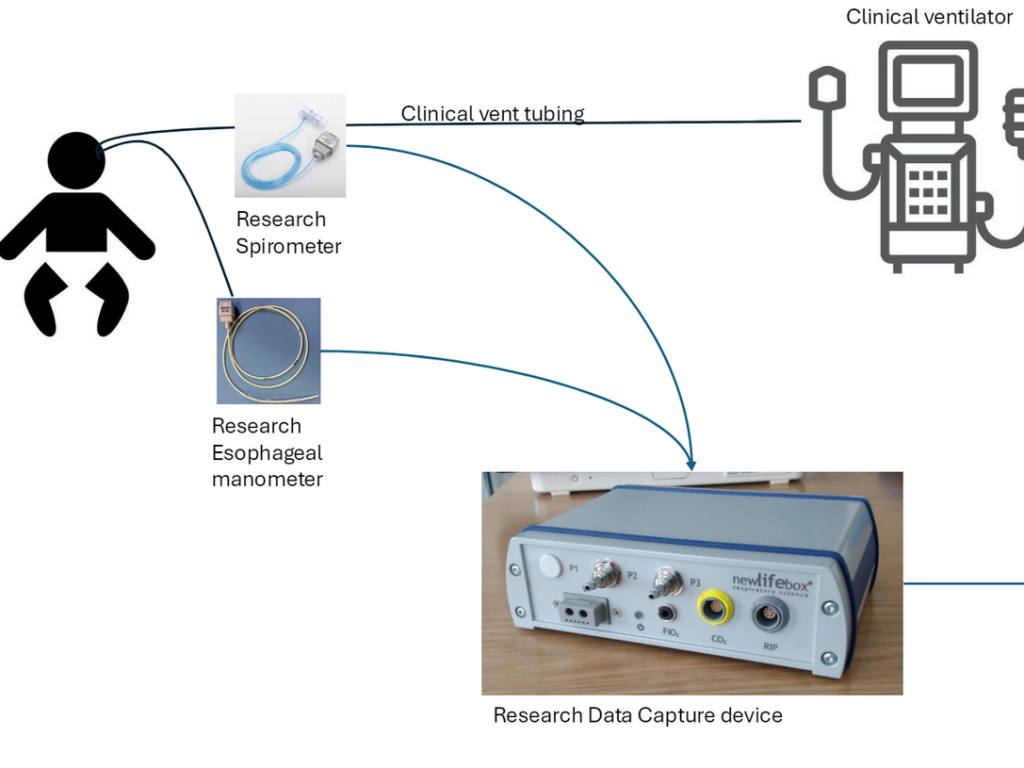
Estimation of Patient Work of Breathing
Esophageal pressure (Pes) measurements can inform mechanical ventilation management. The measured change in Pes (difference between Pes just before the start of inspiration and the lowest Pes during inspiration), or deltaPes, has direct implications on lung stress and work of breathing. Despite these benefits, esophageal manometry is not widely adopted because it involves an invasive catheter that requires expertise in placement and calibration. In collaboration with Drs. Khemani and Yoon, the VPICU is developing a model to estimate deltaPes from commonly available ventilator waveforms: flow and airway pressure.